
Painkillers vs Medical Marijuana for Chronic Pain Management: What 1,450 Patients Told Us
Intro
Prescription painkillers have helped many people, but long‑term use can bring side effects, dependency risks, and diminishing relief. Our 2025 survey of 1,450 patients living with chronic pain reveals how medical marijuana fits into real‑world pain management—how effective patients find it, how often they use it, and whether they reduce or stop other medications after starting cannabis.
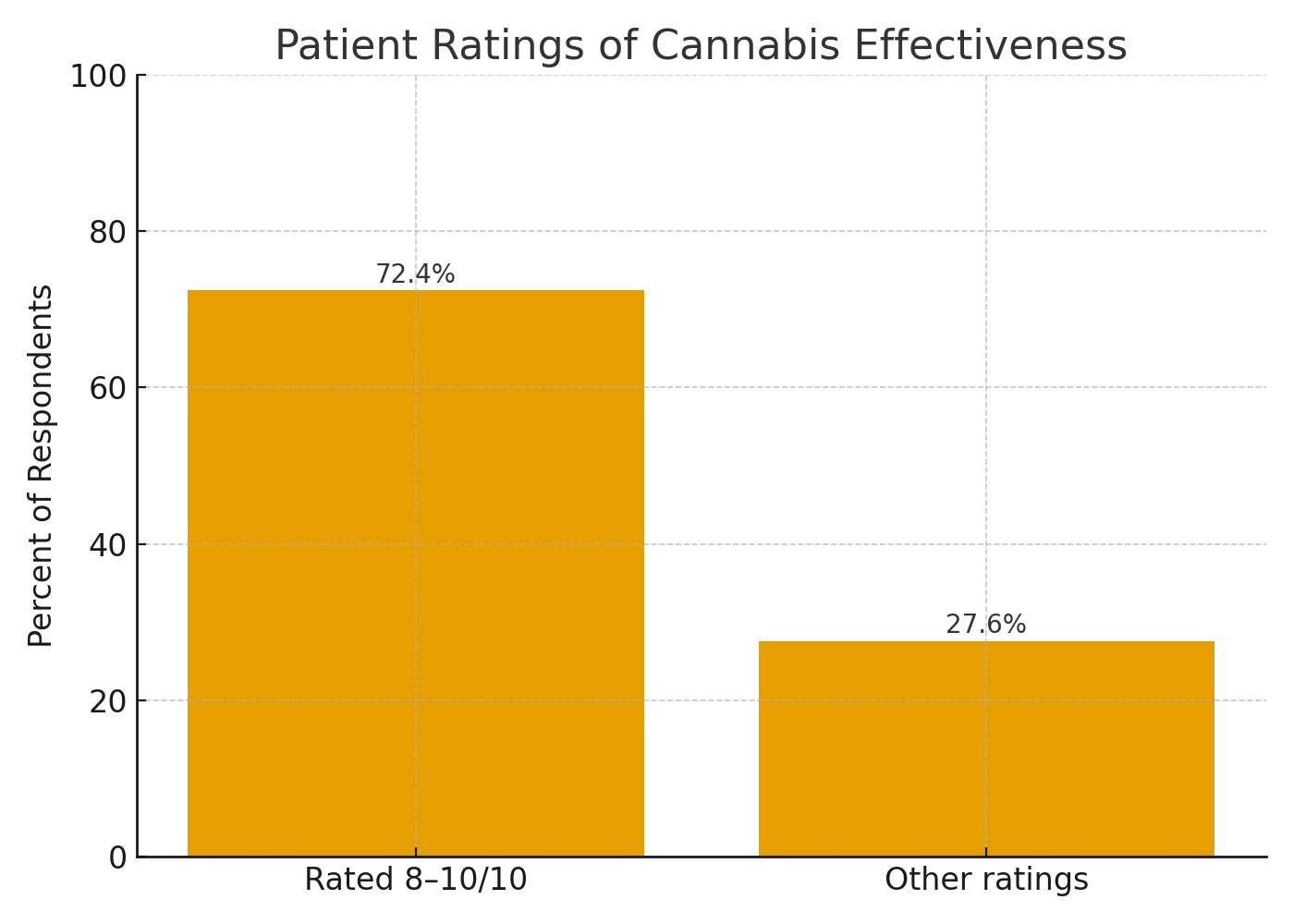
At a glance: 86% report moderate–significant improvement in pain; 72.4% rate cannabis effectiveness 8–10/10; 61.4% reduced or stopped pain pills; 72.7% use cannabis daily.
Download the Full Report
Discover insights based on the survey results of 1,450 medical cannabis patients managing chronic pain.
The Pros and Cons of Medical Marijuana for Chronic Pain (Patient‑Reported)
To compare cannabis with prescription painkillers fairly, it helps to start with how patients actually experience both. Below are the most frequently cited upsides and tradeoffs from our survey, supplemented by common clinical considerations.
Reported Pros of Medical Marijuana
Patients most often cited meaningful pain relief, better sleep, and improved daily functioning. 86% reported moderate–significant improvement, and 72.4% rated effectiveness 8–10/10. Many also value dose flexibility and the availability of formats like tinctures, capsules, and vaporization that let them fine‑tune onset and duration.
Reported Cons and Caveats
Cannabis is not a cure‑all. Some patients reported side effects like dizziness or fatigue, especially with higher‑THC products. Legal frameworks vary by state, product strength may be limited in some programs, and individual responses can differ widely. Careful product selection and physician guidance help mitigate these challenges.
Are Patients Reducing or Replacing Painkillers with Cannabis?
The substitution question—can cannabis reduce reliance on prescription pain medications?—is central for many readers. Our survey offers rare, patient‑level insight into what actually happened after people added cannabis to their regimen.
The Substitution Snapshot
Before cannabis, 48% of respondents were using prescription pain medicines. After starting cannabis: 35% stopped all pain meds, 14.8% stopped some, and 11.6% reduced dose or frequency. Together, that is 61.4% who reported cutting back in some way.
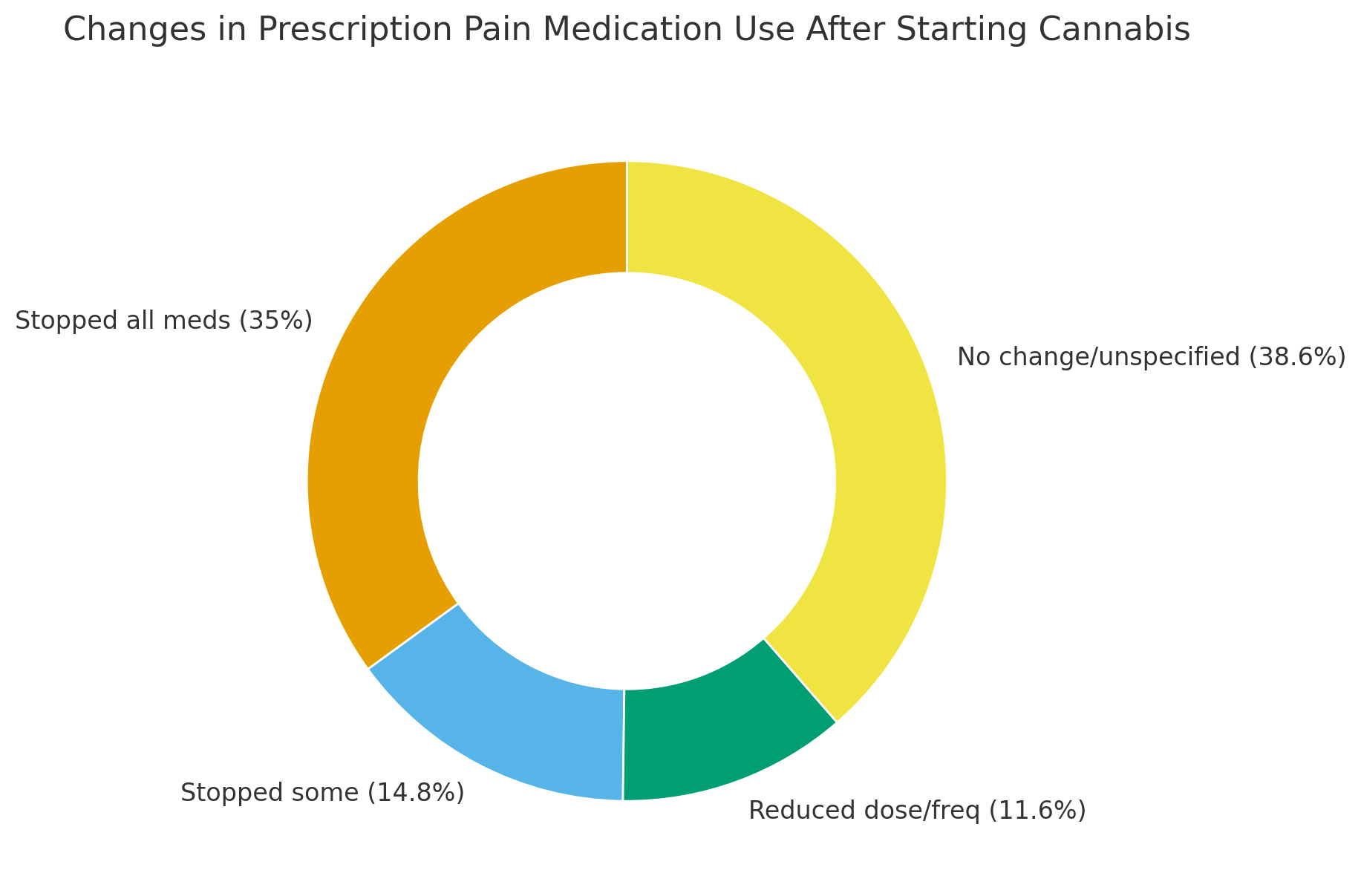
Why Some Still Use Both
A notable share continue a blended plan—using non‑opioid analgesics or carefully managed opioids alongside cannabis. Reasons include targeting different pain mechanisms, covering activity‑related flares, and maintaining continuity while tapering.
What ‘Effective’ Looks Like Day to Day
Effectiveness is more than a number on a scale; it shows up as better nights, easier mornings, and a wider activity window.
High Satisfaction, Consistent Use
72.7% of respondents use cannabis daily, consistent with perceived ongoing benefit. Many describe better sleep quality and fewer overnight awakenings, which can amplify next‑day function.
Sustainable for Long‑Term Conditions
Chronic pain often lasts years. In our sample, 51.5% have lived with pain 10+ years, and 39.3% for 3–10 years. Importantly, 87.8% believe medical marijuana is a sustainable long‑term part of their plan.
Practical Guidance for Safer Transitions
Switching or tapering pain medications should be deliberate and clinician‑guided. The goal is better relief with fewer risks, not a sudden swap.
Start Low, Go Slow, Track
Begin with low‑THC, balanced THC:CBD, or CBD‑forward options and increase gradually. Keep a brief log (pain, sleep, function) to evaluate progress over one to two weeks per adjustment.
Coordinate with Your Prescriber
If you use opioids or other sedating medications, speak with your prescriber before changing doses. A medical cannabis clinician can help craft a taper plan, watch for interactions, and align product choice with your goals.
Side Effects & Safety: How Cannabis Compares to Painkillers
Patients often tell us cannabis side effects feel more manageable than those from long‑term opioids (e.g., sedation, constipation, and respiratory depression risk). With cannabis, the most common issues are transient dizziness, fatigue, dry mouth, or anxiety at higher THC doses. None of this is risk‑free—product choice, dose, timing, and individual history matter. Clinician guidance helps minimize downsides (e.g., starting with balanced THC:CBD, evening dosing, slower titration, or switching formats) while prioritizing safety.
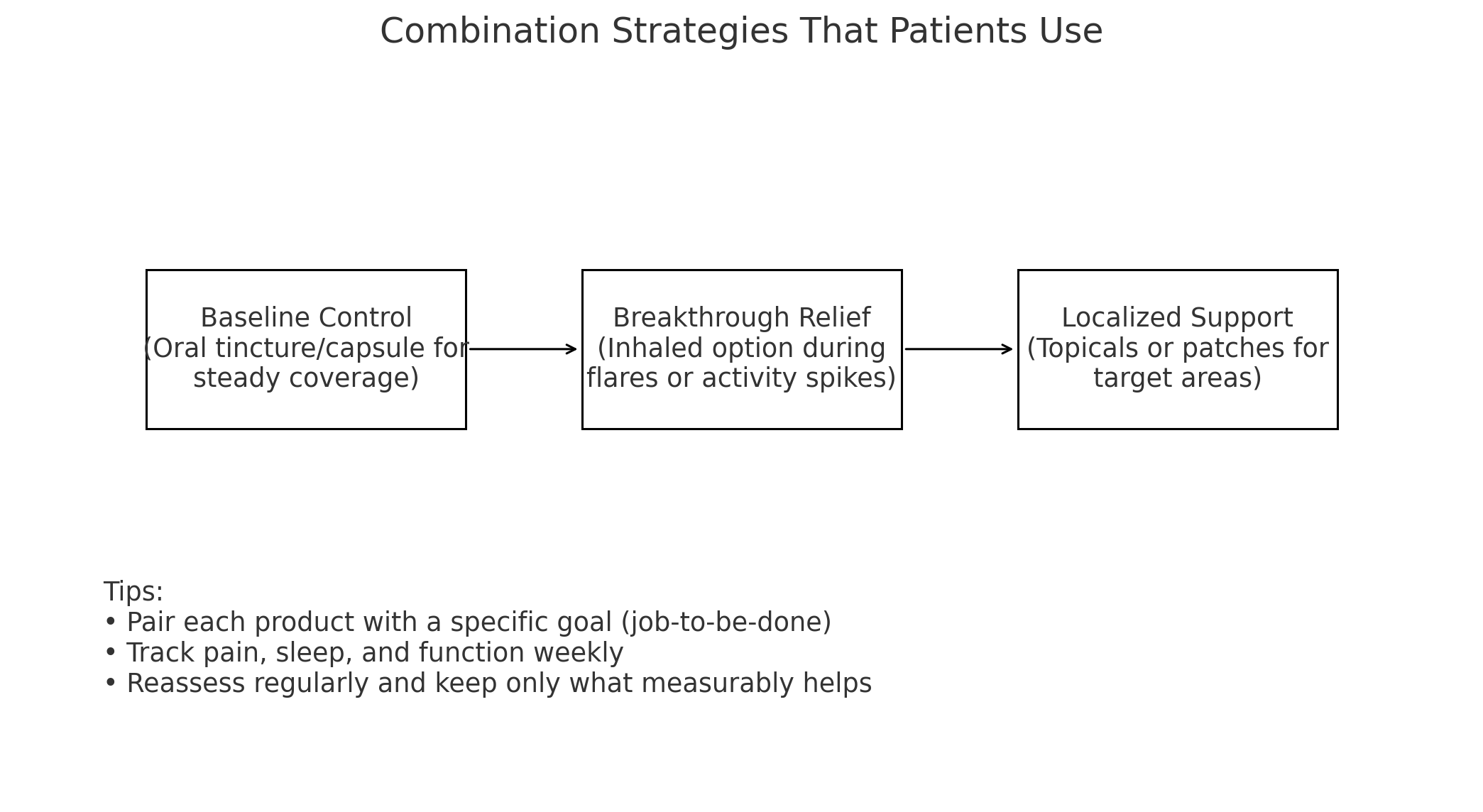
When Patients Use Both: Combination Strategies That Make Sense
Not every patient replaces painkillers outright. Some maintain a blended plan while tapering—or indefinitely—using non‑opioid analgesics for baseline relief and cannabis for flares, sleep disruption, or anxiety that amplifies pain. Others favor a long‑acting oral product for steady coverage and add an inhaled option only during activity spikes. The common thread is intentionality: pair each product with a job‑to‑be‑done, track results, and keep what measurably helps.
Cost & Access Considerations
Costs vary by state, dose, and format. Most patients budget for a physician evaluation plus a monthly product mix (e.g., nightly tincture + small inhaled cartridge for breakthroughs). Over time, some report lower overall spend as prescription copays and adjunct sleep/anxiety meds go down—though this isn’t universal. In low‑THC states, availability can be narrower; ask dispensaries for price‑per‑milligram comparisons so you can evaluate value across options.
Survey Methods & Limitations
This post summarizes self‑reported outcomes from 1,450 patients in 2025. Self‑report can introduce recall or selection bias, and results may not generalize to all pain types or clinical settings. Even so, patient‑level data add essential context that trials often miss—daily use patterns, substitution behavior, and quality‑of‑life changes. Use these findings alongside clinician guidance and current medical evidence.
Download the Full Report
Discover insights based on the survey results of 1,450 medical cannabis patients managing chronic pain.
FAQs about Medical Marijuana for Chronic Pain Management
Is medical marijuana safer than prescription painkillers?
Cannabis has a lower overdose risk than opioids and is not associated with respiratory depression in the same way. That said, it can cause side effects (e.g., dizziness, fatigue), and higher doses of THC may worsen anxiety in some people. Safety comes down to the right product, dose, and medical oversight.
Will cannabis let me stop pain pills entirely?
Possibly. 35% of surveyed patients stopped all prescription pain meds after starting cannabis, and another 26.4% reduced or stopped some. Results vary based on pain type, history, and goals. Work with a clinician to taper safely if appropriate.
Which products work best for steady control vs. flares?
For steady background control, many patients prefer tinctures or capsules for predictable duration. For sudden flares, inhaled products offer faster onset. Topicals and patches can help with localized areas (e.g., joints or back muscles) as an add‑on.
Are there downsides to consider with medical marijuana?
Potential downsides include short‑term side effects, legal variability between states, and product availability differences. Some jobs have workplace policies to consider. Consulting a knowledgeable clinician helps you navigate these issues while maximizing potential benefits.
Will I test positive on a drug test if I use medical marijuana?
Likely yes. Standard workplace and legal drug tests detect THC metabolites, which can remain in urine for days to weeks depending on dose, frequency, and metabolism. If testing is part of your job or custody/medical requirements, speak with your employer or legal counsel and your clinician before starting cannabis. CBD‑only products labeled 0.0% THC still carry some risk of cross‑contamination in poorly regulated markets.
Can I drive or operate machinery while using medical marijuana?
Do not drive or operate heavy machinery while impaired. Even when legally prescribed, driving under the influence is illegal. Plan dosing to avoid peak effects during commute or work hours, and discuss timing strategies with your clinician (e.g., evening dosing, lower‑THC daytime options). Know your state’s per‑se or impairment‑based driving laws.
How fast can I taper off opioids if cannabis is helping?
There is no one‑size‑fits‑all timeline. Safer tapers are gradual and clinician‑guided—often 5–10% dose reductions every 2–4 weeks, adjusted for withdrawal symptoms, pain control, and function. Some patients pause tapers during stressful periods or after procedures. Keep a simple log (pain, sleep, function) to guide pace and product adjustments.
What about tolerance with cannabis?
Tolerance can build with sustained high‑THC dosing. Many patients manage this by using the lowest effective dose, favoring balanced THC:CBD products, rotating formats, scheduling occasional low‑dose days, or emphasizing nighttime dosing. If tolerance becomes an issue, talk with your clinician about structured dose adjustments.

Key Takeaways
- Real‑world relief: Large majorities report meaningful pain reduction and high effectiveness scores with medical marijuana.
- Less reliance on pills: 61.4% reduced or stopped prescription pain meds after starting cannabis.
- Daily use, long‑term fit: Most patients use cannabis daily and view it as sustainable for multi‑year conditions.
- Best outcomes come with guidance: Physician‑guided dosing and product selection improve safety and results.
Related Reading
- What Patients Say About Medical Marijuana for Chronic Pain — Deep dive into survey highlights and quality‑of‑life gains.
- How to Get Medical Marijuana for Chronic Pain in Texas — Step‑by‑step guide to qualifying and filling prescriptions.
- Download the Full Patient Perspectives Report — Methods, charts, and policy insights. (Add final report landing page URL)
- Telemedicine Medical Marijuana Appointments — What to expect and how to prepare. (Add your telemedicine page URL)
Learn More Today!
Considering a change to your pain plan? Book a confidential evaluation with Green Health Docs to discuss a safe, evidence‑informed medical marijuana approach.
 This article has been reviewed by Dr. Anand Dugar, an anesthesiologist, pain medicine physician and the founder of Green Health Docs. Graduating from medical school in 2004 and residency in 2008, Dr. Dugar has been a licensed physician for almost 20 years and has been leading the push for medical cannabis nationwide.
This article has been reviewed by Dr. Anand Dugar, an anesthesiologist, pain medicine physician and the founder of Green Health Docs. Graduating from medical school in 2004 and residency in 2008, Dr. Dugar has been a licensed physician for almost 20 years and has been leading the push for medical cannabis nationwide.
